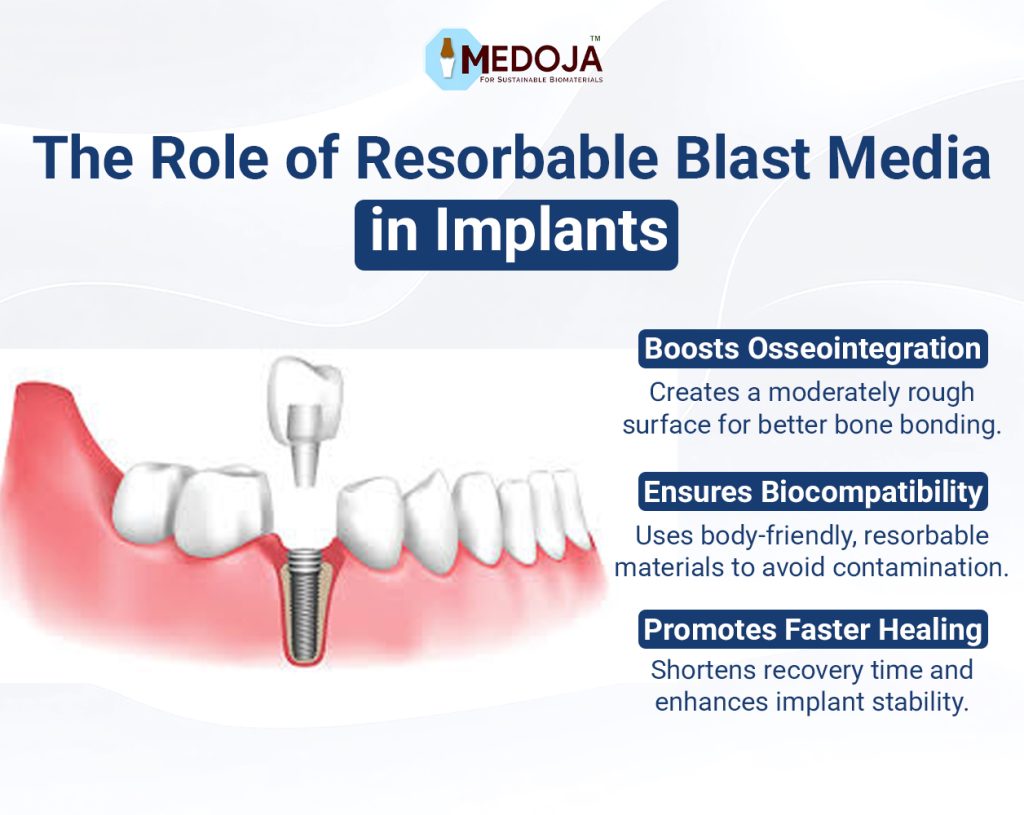
In the evolving world of dental implantology, surface treatment technologies have gained extraordinary attention. A standout among these innovations is Resorbable Blast Media (RBM), a breakthrough that is reshaping how implants integrate with the human body. As dental professionals continually seek improved outcomes, Resorbable Blast Media dental implants are gaining popularity for their ability to enhance osseointegration, promote faster healing, and offer superior long-term stability.
Drawing inspiration from advancements in biocompatible dental materials, much like the significance of hydroxyapatite in biomedical sciences, RBM technology represents a thoughtful synergy between material science and clinical need. But what exactly is Resorbable Blast Media? Why has it become so important in dental implant surface treatment? And how does it compare to other technologies like SLA (Sandblasted, Large grit, Acid-etched) treatments?
Let’s dive deep into the world of RBM and explore its role in modern bone implant surface technology.
Resorbable Blast Media refers to a specialized technique for treating the surface of dental implants. In RBM treatment, the implant surface is blasted with biocompatible, resorbable particles, typically calcium phosphate-based materials at high speeds to create a moderately rough texture.
What sets RBM apart from traditional blasting materials (like alumina) is its ability to dissolve safely in the body over time. Since the blasting media is made from substances the body can naturally resorb, there’s no risk of contamination or inflammatory response, ensuring greater biocompatibility and improved osseointegration in dental implants.
In short, RBM-treated implants combine precision engineering with biological harmony, making them a preferred choice for clinicians focused on long-term success.
Before understanding why RBM stands out, it’s essential to recognize why surface treatment matters in implants.
Dental implants are essentially foreign objects placed into bone. For successful integration, the implant surface must encourage the growth of new bone tissue — a process known as osseointegration. Smooth surfaces often struggle with achieving strong bone bonds. However, when implants are moderately roughened through techniques like RBM, they provide a larger surface area for bone cells (osteoblasts) to adhere, proliferate, and integrate.
This is where surface roughness in dental implants becomes critical. An optimized roughness enhances mechanical interlocking between bone and implant, shortens healing times, and improves load distribution leading to stronger, more durable results.
The RBM process involves:
The result is an implant surface that is:
Compared to untreated or polished surfaces, RBM surfaces dramatically improve bone anchoring, reduce the risk of implant failure, and promote quicker patient recovery.
Both RBM surface implants and SLA implants are highly respected in dental practice, but they differ subtly:
| Aspect | RBM Implants | SLA Implants |
| Surface Material | Calcium phosphate (resorbable) | Alumina blasting + acid-etching |
| Roughness Level | Moderate roughness | Higher roughness (macro and micro) |
| Biocompatibility | High (resorbable, body-friendly) | High (but with potential residual acid) |
| Risk of Contamination | Very low (due to resorbable media) | Slight if not properly processed |
| Healing Time | Fast | Very fast |
| Clinical Applications | Ideal for standard cases | Preferred for complex cases (e.g., soft bone) |
Both have their place depending on case complexity, but RBM dental implants are often considered safer for general use due to the absence of residual blasting material and superior biological acceptance.
Several factors make RBM dental implant technology highly attractive:
The future of bone implant surface technology lies in multifunctional surfaces — ones that not only encourage osseointegration but actively resist infection, enhance regeneration, and even release therapeutic agents.
Research is exploring ways to combine RBM treatments with nanotechnology to create nanostructured RBM surfaces that mimic natural bone even more closely. Innovations in biocompatible dental materials also point towards integrating growth factors directly into implant surfaces, potentially revolutionizing patient outcomes.
As we move forward, RBM surface implants could be further enhanced by blending resorbable nanoparticles, bioactive coatings, and customized surface roughness profiles tailored to individual patient needs.
To conclude, the role of Resorbable Blast Media (RBM) in implants marks a transformative chapter in dental implant surface treatment. By combining mechanical stability with biological wisdom, RBM-treated implants offer unparalleled performance in promoting osseointegration, minimizing contamination, and ensuring patient satisfaction.
When evaluating choices like RBM vs SLA implants, it’s clear that RBM offers unique advantages in terms of purity, compatibility, and simplicity, making it a compelling choice for modern implantology.